30
An approach to reviewing a chest x-ray will create a foundation that will facilitate the detection of abnormalities. You should create your own strategy. There is no correct way to analyze the images. Consistency and thoroughness are good general strategies. With time, and repetition, the process will become subconscious. Repetitive viewing of images will help establish a baseline of normality and normal variation that will represent an internal yard stick for the detection of variation from normal.
Detection of abnormality will allow you to diagnose clinical conditions that may require medical attention. Remember, abnormalities on imaging are simply aberrations of anatomy.
For example, a numerical strategy can be deployed:
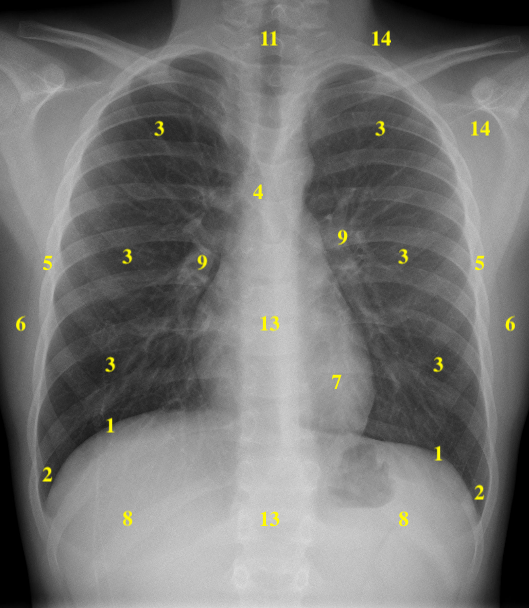
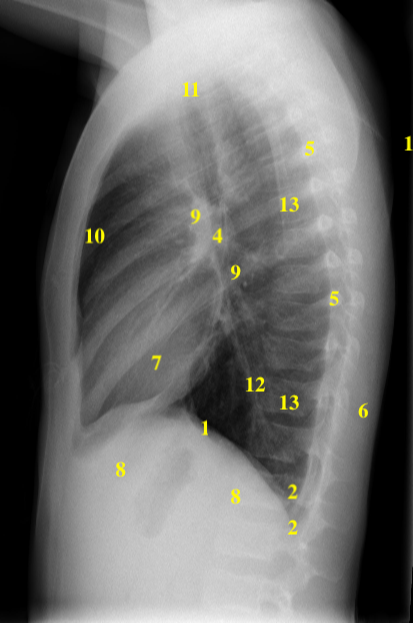
| 1 | Hemidiaphragms | 8 | Below Hemidiaphragms |
| 2 | Costophrenic Angles | 9 | Hila |
| 3 | Zones of the Lungs | 10 | Anterior Mediastinum and Sternum |
| 4 | Carina and Bronchi | 11 | Trachea |
| 5 | Pleura and Ribs | 12 | Posterior Mediastinum |
| 6 | Chest Wall | 13 | Spine |
| 7 | Cardiac Silhouette | 14 | Soft Tissue of the Axilla and Lower Neck |
Terminology Pertinent to the Chest x-ray:
| Term | Definition |
| Lucency | Darker area on the image as relatively more of the administered x-rays reaching the detector |
| Opacity | Whiter area on the image due to absorption of the x-rays prior to reaching the detector |
| Consolidation | Process by which air in the lungs is replaced by products of disease rendering the lung more solid |
| Nodule | Opacity < 3 cm in diameter |
| Mass | Opacity > 3 cm in diameter |
| Line | Linear opacity < 2 mm in thickness |
| Stripe | Linear opacity 2 – 5 cm in thickness |
| Hilum | Singular |
| Hila | Plural |
| Hilar | Adjective |
Table 5.1 Terminology pertinent to chest x-ray
1)Chest x-ray Image Acquisition Positioning:
Posterior-Anterior (PA):
Lateral:
2) Assess Image Quality:
Acronym: ‘RIPE’:
| Rotation | The medial aspect of each clavicle should be equidistant from the vertebral spinous processes |
| Inspiration | Adequate inspiration is when:
5 – 6 anterior ribs, 9 – 10 ribs posteriorly in the mid-clavicular line, the lung apices, both costophrenic angles and the lateral rib edges are all visible |
| Projection | AP vs. PA film |
| Exposure | Left hemidiaphragm visible to the spine and vertebrae visible behind the heart |
Alterations in standardized positioning, or x-ray exposure, will alter the ‘typical’ appearance of the image and may lead to inaccurate assessment, or misdiagnosis.
Ensure laterality is correct i.e. the Right (R) or Left (L) marker should correspond to proper anatomic orientation, e.g. liver on the right, etc.
3) Chest X-Ray – ABCDE Approach
A – Airways/Mediastinum:
Airways
The trachea is normally located centrally or just slightly to the right of midline.
If the trachea is deviated, look for anything that could be pushing or pulling the trachea.
Pushing of trachea – e.g. large pleural effusion / tension pneumothorax / mediastinal mass
Pulling of trachea – e.g. lobar collapse, lung fibrosis
Rotation of the patient can give the appearance of a deviated trachea, so as mentioned above, check the clavicles to rule out rotation as the cause.
Carina
The carina is located at the point at which the trachea divides into the left and right main bronchus. On a good quality CXR this division should be visible. This division creates a carinal angle. This bifurcation of the trachea is an important landmark when assessing nasogastric tube placement, as the NG tube should pass distal to the carina in a vertical, midline, orientation.
Bronchi
The right main bronchus is generally wider, shorter, and more vertically oriented than the horizontally oriented, longer, left main bronchus. As a result, it is more common for inhaled foreign objects to become lodged in the right side bronchial tree as the route is more direct. Depending on the quality of the CXR, you may be able to see the main bronchi branching into further subdivisions of bronchi which supply each of the lungs lobes.
Mediastinum
Paratracheal stripes
Right thicker than left, should have smooth contours. Lobulation of the contour of the paratracheal region suggests mass(es) or lymphadenopathy.
Mediastinal contours
The mediastinum contains the heart, great vessels, lymphoid tissue, major airways, and a number of potential spaces where pathology can occur. The lung – soft tissue boundary of the mediastinum on a CXR is a very important relationship to assess. This lung – soft tissue boundary is caused by the contrast between the predominantly air filled lung against the soft tissue of the mediastinum. This allows one to determine if an abnormally large, or bulging mediastinal contour is present or if an assortment of smaller bulges can be seen related to hilar or mediastinal lymph nodes or enlarged vessels.
If the lung opacity adjacent to the mediastinum is different (pneumonia, atelectasis, interstitial markings) this may partially, or completely, obscure the normally expected distinctive, smooth mediastinal interface, this is called the “Silhouette sign”. Gas in the mediastinum (pneumomediastinum) and gas in the pleural space (pneumothorax) will also alter the appearance of the mediastinal contours as the gas will be lucent. Pleural fluid (effusion) can obscure mediastinal anatomy if it accumulates in the vicinity.
Aortic knob
Left lateral edge of the aorta as it arches back over the left main bronchus.
Loss of definition and/or enlargement of the aortic knob contour is abnormal.
Aorto-pulmonary window
The aorto-pulmonary window is a space located between the arch of the aorta and the left pulmonary artery. This space can become opaque and may have an outward convex margin, as a result of mediastinal lymphadenopathy (e.g. malignancy).
Hilar structures
The hila consist of pulmonary vasculature, lymph nodes, fat, and the major bronchi.
The left pulmonary artery branch is more vertical and is a visible component of the left hilum while the right is more horizontal and not seen.
The left hilum is often positioned slightly higher than the right (97%), it is also more posterior on the lateral view, but there is variability.
The hila are usually roughly the same size, so asymmetry should raise suspicion of pathology.
Hilar enlargement can be caused by a number of different pathologies: bilateral symmetrical enlargement can be seen in sarcoidosis or lymphoma. Unilateral / asymmetrical enlargement may be due to underlying lung malignancy.
B – Breathing:
Lungs
You can divide each lung into 3 zones, each occupying 1/3 of the height of the lung.
Alternatively, one can create 3 imaginary zones radiating from the hilum i.e. inner zone with larger caliber vessels and bronchi, mid-zone with medium sized vessels, and the outer zone with small vessels. These zones do not equate to lung lobes.
Inspect each zone, ensuring that appropriately sized lung markings occupy the zone. Assess for asymmetry. The vessels in the lungs are larger in the lower lobes, normally.
Review the lung apices as there may be hidden pathology obscured by the clavicles and ribs.
Increased opacity in an area of the lung may suggest pathology (e.g. consolidation / nodule / mass). The absence of lung markings within a segment of the lung should raise suspicion of pneumothorax or severe emphysema.
Some pathology can cause symmetrical changes in the lung, making it more difficult to recognize, so it’s important to keep this in mind (e.g. pulmonary edema).
Pleura:
The pleura are not normally visible in healthy individuals. The pleural surface should be smooth and parallel the rib cage. Fluid (hydrothorax) or blood (hemothorax) can also accumulate in the pleural space, causing an area of increased opacity. As fluid tracks up the wall of the chest in the pleural space it creates a meniscus just as water does in a beaker.
C – Cardiac:
Cardiac silhouette size (heart size)
The cardiac silhouette should occupy 50%, or less, of the thoracic width (e.g. a cardiothoracic (CTR) ratio of <0.5).
This rule only applies to PA chest x-rays (AP films exaggerate cardiac silhouette size), so you should not draw any conclusions about heart size from an AP film.
If the heart occupies more than 50% of the thoracic width (on a PA CXR) then this suggests enlargement. Enlargement of the cardiac silhouette can occur in a wide variety of conditions including, heart valvular disease, cardiomyopathy, pulmonary hypertension and pericardial effusion.
Assess heart borders
Inspect the borders of the heart which should be well defined in healthy individuals:
The heart borders may become difficult to distinguish from the lung as a result of various pathological processes (e.g. consolidation) which cause increased opacity of the lung tissue. (The silhouette sign)
The right atrium makes up most of the right heart border. The left ventricle makes up some of the left heart border, with a contribution for the left atrium.
Loss of definition of the right heart border is associated with right middle lobe consolidation
Loss of definition of the left heart border is associated with lingular consolidation
D – Diaphragm:
The right hemidiaphragm is in most cases higher than the left (as a result of the underlying liver). The stomach underlies the left hemidiaphragm and is best identified by the gastric air bubble located within it.
The diaphragm should be indistinguishable from the underlying liver in healthy individuals on an erect CXR, however if free gas is present (often as a result of bowel perforation), air accumulates under the diaphragm causing it to elevate and become visibly separate from the liver.
Costophrenic angles
The costophrenic angles are formed from the dome of each hemidiaphragm and the lateral chest wall.
In a healthy individual the costophrenic angles should be clearly visible on a normal CXR as a well defined acute angle.
Loss of this acute angle (referred to as costophrenic blunting) can suggest the presence of fluid, scarring, or consolidation.
E – Etcetera:
Bones – alignment, fractures, lytic or sclerotic lesions. Follow the ribs bilaterally, view the spine and sternum on the lateral view.
Soft tissues – bulging contours, unusual opacities (mass) or lucencies (mastectomy).
Iatrogenic – tubes, catheters, pacemakers, etc.
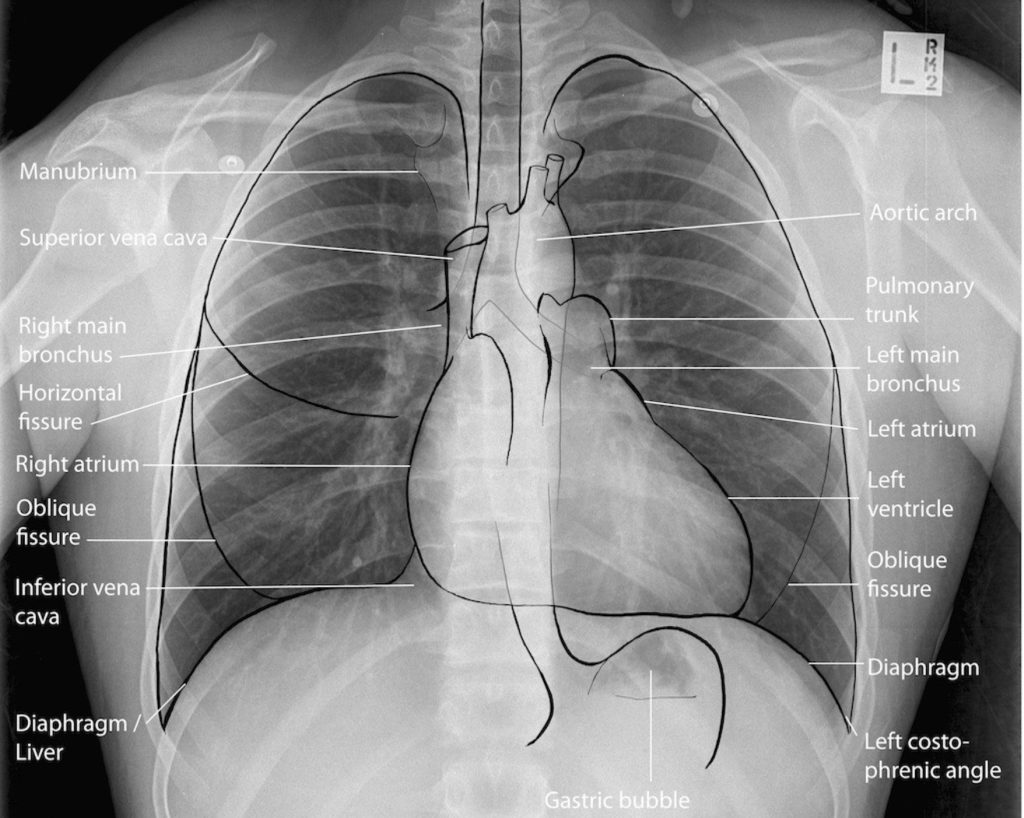
5) Line Drawing – AP Chest X-ray
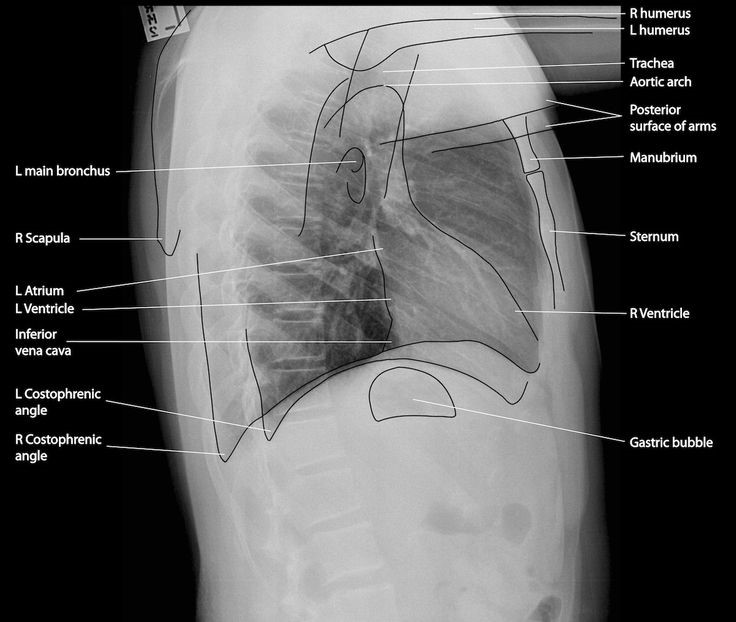
6) Line Drawing – Lateral Chest x-ray
Attributions
Fig 5.3 A Numerical system for Chest x-ray review by Dr. Brent Burbridge MD, FRCPC, University Medical Imaging Consultants, College of Medicine, University of Saskatchewan is used under a CC-BY-NC-SA 4.0 license.
Fig 5.4 Positioning for a PA Chest x-ray, by the Distance Education Unit, University of Saskatchewan, is published using a CC-BY-NC-SA 4.0 International License.
Fig 5.5 Positioning for a Lateral Chest x-ray , by the Distance Education Unit, University of Saskatchewan, is published using a CC-BY-NC-SA 4.0 International License.
Fig 5.6A Line Drawing of AP Chest x-ray by Line drawings – #FOAMed Medical Education Resources by LITFL is licensed under a CC-BY-NC-SA 4.0 License.
Fig 5.6B Line Drawing of Lateral Chest x-ray by Line drawings – #FOAMed Medical Education Resources by LITFL is licensed under a CC-BY-NC-SA 4.0 International License.
